
Center for Traumatic Brain Injury Research
Individuals with traumatic brain injury (TBI) can have difficulty in their daily lives because of persistent deficits in their abilities to think, learn, and remember. These complications can interfere with participation in school, work, and community activities, hamper caregiving, and negatively impact overall quality of life. Through research, we develop new ways to help individuals with TBI recover cognitive function and mobility to live better lives.
Center Leadership
Center Leadership
-

-

Associate Director, Neuropsychology Research
-

Assistant Director, Neuroscience Research
Center for Traumatic Brain Injury Research
Laboratory Leadership
Laboratory Leadership
-

Senior Research Scientist
-

Senior Research Scientist
-

Northern New Jersey Traumatic Brain Injury System
The Northern New Jersey Traumatic Brain Injury System (NNJTBIS) fosters collaborative research that addresses the lifelong needs of the TBI community. NNJTBIS translates findings into clinical care and provides resources for individuals with TBI and their caregivers. NNJTBIS is designated as a federally funded Traumatic Brain Injury Model System and one of only 16 TBI model systems in the U.S.

Breaking New Ground with Exploratory Interventions
Center research teams are assessing results of several TBI-focused clinical studies: the cognitive effects of aerobic exercise on people with significant memory loss; what happens in the brain after a person learns new information; how a 45-minute nap can help improve daily movement-related tasks; and if a balance-training program can help people with TBI avoid falls.
Join a Study
Aerobic Exercise and Memory Brain and Learning Motor Learning and Sleep Avoiding Falls after TBI

Applying Virtual Reality Technology to Rehabilitation Research
Virtual reality (VR) technology offers a new approach to engaging individuals with TBI in interactive programs aimed at improving cognitive and physical function. Collaborative studies are underway using immersive VR tools for assessing cognitive function, treating cognitive impairments, and improving balance deficits. As our understanding of the cognitive consequences of TBI continues to expand, so does the potential for effective treatment.

Teaching Context and Imagery to Facilitate Learning in TBI
To improve a person’s ability to learn and remember new information, researchers here established a memory retaining treatment protocol using context and imagery. This cost-effective, drug-free, computer methodology is called Kessler Foundation modified Story Memory Technique (KF-mSMT®). Ongoing studies show significant improvement in persons with TBI, especially on memory tasks. KF-mSMT was developed by Nancy Chiaravalloti, PhD, and team. It is available for clinical use in English and Spanish.
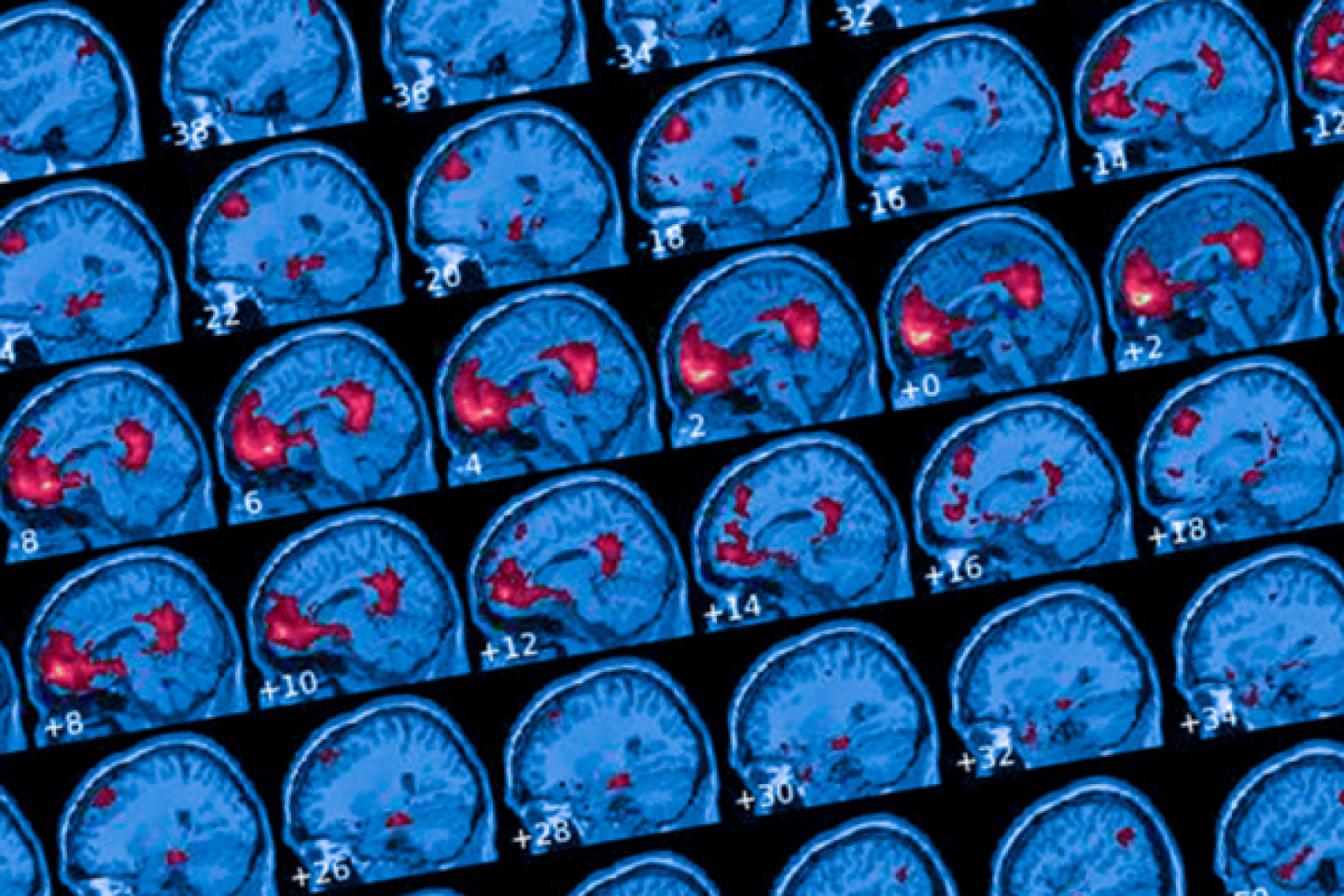
Combatting Disabling Cognitive Fatigue with Neuroimaging
Individuals with neurological damage often report a lack of mental energy, called cognitive fatigue, that interferes with their ability to perform daily activities. Using neuroimaging techniques, researchers are learning more about the underlying mechanisms of cognitive fatigue in TBI, which is fundamental to the development and testing of new behavioral interventions.

Enhancing Quality of Life for Caregivers and Patients
TBI and dementia are common causes of long-term disability and caregiver burden. Many existing services help the family in the moment, but do not address long-term wellness. Researchers are testing the effectiveness of group wellness treatments designed to teach coping and management skills to each patient and caregiver pair. This approach will position each pair to work as a team and gain the skills they need to adapt to the challenges of daily living. (Study is in development.)
Exploring Treatments for Long-term Memory Impairment
Because TBI can result in considerable difficulty in learning and remembering new information, researchers are taking initial steps to develop process-specific treatment strategies. They hope to clarify the dysfunctional cognitive and neural processes that underlie memory loss in TBI. These discoveries will potentially lead to developing new TBI therapies where little evidence-based treatment exists.
Multimedia

You Help Annie Regain Strength in Body and Mind
After Annie Modica sustained a traumatic brain injury (TBI) in a car accident, doctors predicted that she would never have full use of her arm again. With the support of our donors, Annie joined a Kessler Foundation research study to regain strength and independence on her journey to recovery.
Now, her confidence is lifted and she is back to enjoying her active family life.
To learn more about TBI, read additional reference materials and links we’ve compiled.

Join a Research Study Today